Our Work
Last Updated: Wednesday, 21 January 2026North Liverpool Primary Care Network is the provider of a number of workstreams. Read the information below to find out more about our work.
Commissioned Services
Digital Team
The Primary Care Network Digital Team supports both the Primary Care Network and GP practices to improve health and wellbeing by utilising data to identify those in need of support or targeted interventions, improving processes for capturing and using information and supporting practices with any digital requirements.
The team also work on projects such as improving capacity and access to ensure patients are seen appropriately and quickly, how to best utilise technology to create smoother patient pathways and testing new technologies and software.
Enhanced Health in Care Homes
We have an ambition for the NHS to strengthen its support for the people who live and work in and around care homes. People living in care homes should expect the same level of support as if they were living in their own home – but this can only be achieved through collaborative working between health, social care, voluntary, community, and social enterprise
- every care home being aligned to a named PCN
- every care home having a named clinical lead
- a weekly ‘home round’ or ‘check in’ with residents prioritised for review based on MDT clinical judgement and care home advice (this is not intended to be a weekly review for all residents)
- within 7 days of re/admission to a care home, a resident will have a person-centred holistic health assessment of need (will include physical, psychological, functional, social and environmental needs of the person and can draw on existing assessments that have taken place outside of the home, as long as it reflects their goals)
- within 7 days of re/admission to a care home, a resident will have in place personalised care and support plan(s), based upon their holistic assessment
This programme is supported by our work to ensure that Urgent Community Response is accessible to people living in a care home, increased support for nurses working in care homes through a national network, and the appointment of a chief advisor on care home nursing. Information will also be shared more easily and securely between the NHS and care homes, with NHS mail, now available to all care homes. It also supports video conferencing, enabling a virtual home round if necessary.
Multidisciplinary teams’ role in enhancing the health of care home residents
A new animation shows how multidisciplinary teams can work together to improve the health of residents, and work with them to plan their proactive and personalised care.
This animation brings together professionals from a health and social care setting in a multidisciplinary team, highlighting the various roles they play, and how, together, they help ensure that residents receive the additional care they need.
All care homes should be connected to the Enhanced Health in Care Homes Service, including those who support working age adults, not just older people.
For more information please visit
NHS England » Enhanced health in care homes
The team consists of the following at the minute:
Dr Velayudham Murugesh - Clinical Lead for Care Homes
Julie - Care Home Co-ordinator
Dr Pooja
Dr Arvind
Francesca
Wellbeing Link Workers
Wellbeing Link Workers help give you the time to find ‘what matters to you’, we can link you to a wide range of community resources that can help with:
Mental Wellbeing
Social Activities
Benefits advice
Housing
Education
Family/carers
Physical activity
and more...
The goal is to develop a wellbeing plan by identifying the cause of your problem and linking you with the most suitable support to help improve your wellbeing.
Wellbeing Link Workers are not support, social workers, counsellors or mental health specialists.
Meet the Team:
Rebecca G
Rebecca M
Julie J
Noor
Joseph
Melanie
Nicola
Mark
Ter
Julie L
For the latest updates, please follow the North Liverpool Network Link Worker Team on twitter.
Click here to visit their page
To book an appointment please contact your GP
Pharmacy Team
A Primary Care Network (PCN) pharmacist works alongside a multidisciplinary diverse team of health care professionals in general practice and within the primary care network, providing primary support for prescription and medication queries.
As a PCN pharmacist you will take responsibility for medicines optimisation within the PCN, medicines reconciliation, the provision of expert advice on clinical medicines and the undertaking of structured clinical reviews with patients to proactively manage their complex polypharmacy needs.
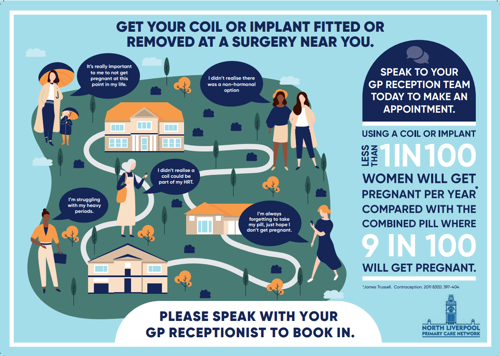
Womens Health Hub
The North Liverpool PCN’s ‘Women’s Health Hub’ has been in operation since 2020 and aims to improve access to women’s services in the local area. The Liverpool model was featured in the Women’s Health Strategy and is now a leading example for other areas creating similar services.
What do we offer?
We provide several services to patients within our network. These include insertion and removal of LARC (Long-Acting Reversible Contraception, like coils and implants) after an initial phone consultation. We also offer ring pessary insertions and changes, alongside a monthly Saturday Smear clinic. Additionally, we have a specialist a HRT service and can answer more general women’s health inquiries in our telephone clinic.
How can I access the service?
Our service operates predominantly from the Croxteth Family Health Clinic (L11 0BS). If your GP is in the North Liverpool PCN, you can access any of our services by simply speaking to your GP receptionists and they should be able to book you in (subject to availability). Alternatively, you can fill in one of our self-referral forms online and we will give you a call:
Smear Request Form (once a month Saturday clinic - appointments limited)
Cancer Screening
Cervical Cancer Screening
Cervical cancer screening (smear tests) are used to detect early signs of cervical cancer in women. The screenings help to identify abnormal cells that may eventually lead to cancer, allowing for early intervention and treatment. The most common screening test is the smear, which involves checking the cervix (the neck of the womb) for the presence of human papilloma virus (HPV). Screening may detect abnormal cells before they turn into cancer, and regular screening can prevent cancer from developing. It is recommended that anyone with a cervix between the ages of 25 and 64 get screened for cervical cancer regularly. Appointments for your smear tests can be booked through your GP. For more information on cervical screening visit Cervical screening - NHS (www.nhs.uk).
Breast Cancer Screening
Breast cancer screening is the best way to detect breast cancer early, before symptoms developed. The most common screening test for breast cancer is a mammogram, which uses X-rays to create images of breast tissue. It is recommended that women between the ages of 50 and 71 attend screenings every 3 years, and women who are classed as high risk for breast cancer (such as those with a family history of the disease) may need to begin screening earlier and attend appointments more frequently. In addition to mammograms, women should perform self-examinations on their breasts and report any changes in their breast tissue to their GP. More information on this can be found here: Check your breasts | Breast Cancer UK.
Mammograms are not perfect and some cancers will not be visible, which is why it is essential for women to be familiar with their own breasts and report any changes. For more information on breast screening visit Breast screening (mammogram) - NHS (www.nhs.uk). You can call 0151 282 6920/6921 or email bscreening@rlbuht.nhs.uk to book your breast screening.
Bowel Cancer Screening
Bowel cancer screening is a way to detect early signs of colon or rectal cancer, also known as colorectal cancer. . The most common screening test for bowel cancer is a faecal immunochemical (FIT) test, which looks for hidden blood in the stool. Bowel cancer screening can detect early signs of cancer before symptoms develop, and regular screenings can help prevent cancer from developing. It is recommended that adults aged 60-74 years old should participate in bowel cancer screening every 2 years. Some people may have an increased risk of bowel cancer due to genetic or lifestyle factors and may require earlier and more frequent screening. To order you bowel screening kit please contact 0800 707 60 60. For more information on bowel screening visit Bowel cancer screening - NHS (www.nhs.uk). You can order your bowel screening kit by calling the helpline on 0800 707 60 60.
Severe Mental Illness
What is Severe Mental Illness?
Severe mental illness (SMI) refers to psychological problems, such as schizophrenia, bipolar and psychosis, that often lead to an impaired ability to engage in functional and occupational activities.
Why is it Important to Attend Physical Health Checks?
Many people with a severe mental illness experience at least one physical health condition alongside their mental illness and have a higher prevalence of health issues such as obesity, asthma, diabetes, chronic obstructive pulmonary disease (COPD) and hypertension. By attending your annual physical health check, clinicians are able to identify any issues and reduce these health inequalities.
How can North Liverpool Primary Care Network Help?
At North Liverpool PCN, our aim is to improve engagement to physical health checks for SMI patients. Our Care Coordinators are here to provide support and remove any barriers that may be preventing you accessing your appointments. By making reasonable adjustments prior to your appointment or signposting to organisations and resources for support, we can take the right steps to improve your physical health.
Health and Wellbeing
At North Liverpool PCN, our Health and Wellbeing Coaches are available to offer support and guidance on a range of issues regarding your physical and mental health.
What is a Health & Wellbeing Coach?
- Health & Wellbeing Coaches create a safe, thinking environment for you to discuss your lifestyle and any changes you may want to make to improve your health & wellbeing.
- Initial consultations can take up to 60 minutes and will discuss your lifestyle holistically whilst focusing on four main aspects, including your food choices, movement, relaxation techniques and sleep.
- Health & Wellbeing coaches will support you in achieving your goals and provide you with information and resources to help you on your journey.
- Support is varied and can range from helping you with diabetes and weight management, cholesterol and blood pressure to anxiety, and sleep support.
- Seeing a Health & Wellbeing coach can be therapeutic for people, but it is not therapy, instead it is a way to look forward and make positive lifestyle changes. If you feel you need further support, wellbeing referrals can be made to our Social Prescribing Team. Please ask for more information at your appointment.
Who can access the service?
Anyone over the age of 16 years who is registered at one of the GP surgeries listed below can access the service. You can self-refer by contacting reception or by completing an e-consult or you can be referred by your GP or a member of the Health Care Team.
How can I book an appointment?
To self-refer, please contact the surgery directly via telephone on the numbers below. Please note phone lines are less busy during the afternoon. Health & Wellbeing Coaches are available on the days listed next to the GP surgeries.
What is a healthy lifestyle?
Good health is about the absence of disease and illness and a healthy lifestyle means practicing daily activities and habits to encourage physical, mental, and spiritual wellbeing. Daily activities and habits should be centred around the foods you eat, the way you move, how well you sleep and how much you relax. Our bodies are machines that require regular nutrients, hydration, and rest, to run efficiently. Without this balance your health and wellbeing will suffer.
Our lifestyle effects our health and should be treated with a holistic approach balancing our food, movement, sleep, and relaxation. Small changes to our daily lives can help keep us in a balanced state and prevent further illness. Our lifestyle is simply about what we do and our way of living, and our health and wellbeing is about being and feeling healthy and happy with the absence of disease.
Healthy Lifestyle Tips
- Eat mostly real foods and reduce the amount of ultra-processed food from your diet; most of your food should be from fruit, vegetables, nuts/seeds, beans/pulses, eggs, vegetable oils, herbs/spices, wholegrains, meat fish and dairy and should not be pre-prepared.
- Drink mostly water; aim for at least 1 litre of water a day and avoid ultra-processed drinks such as carbonated drinks, energy drinks, flavoured coffees, smoothies and milkshakes.
- Reduce your caffeine intake after midday; to help improve your sleep quality.
- Do some sort of physical activity every day; engage in a mixture of aerobic and resistance exercises for as little as 10 minutes each day.
- Get at least 6 hours of sleep each night; your sleep is so important to help restore your brain and body each night and sleep quality is just as important as sleep quantity.
- Allow yourself to switch off and do something you enjoy and find relaxing every day; learn to wind down and reduce your stress and anxiety by practicing a daily mindful activity.
- Aim to drink no more than 14 units of alcohol each week; have some nights alcohol free. A regular bottle of wine is approximately 10 units and an average pint of beer is about 2 units.
- Avoid smoking or any other harmful substances.
“If you really want to do something you will find a way, if you don’t, you’ll find an excuse.” – Jim Rohn
Learning Disabilities
What Defines a Learning Disability?
A learning disability is lifelong condition and is different for everyone. The Department of Health and Social Care (2001) define a learning disability as "a significantly reduced ability to understand new or complex information, to learn new skills (impaired intelligence), with a reduced ability to cope independently (impaired social functioning), which started before adulthood.". The degree of disability can vary significantly, ranging from mild, moderate, severe or profound.
Annual Physical Health Checks
Everyone who is over 14 years old and on their doctors learning disability register qualifies for an annual health check. During your physical health check you will:
- get a physical check up, including height, weight, blood pressure, heart rate
- have your blood and urine tested
- talk to you about staying well and if you need any help with this
- talk to you about your medicines to make sure you are being given the right medicines when you need them
- check to see if your vaccinations are up to date
- check how you are feeling if you have a health problem such as asthma or diabetes
- check to see if you have any other health appointments
- ask if your family or carers are getting the support they need
- help make sure that things go well when children move to adult services at the age of 18
At North Liverpool PCN we aim to make access to the GP as easy as possible. We can arrange and provide reasonable adjustments, such as longer appointments or beginning or end of the day appointments to avoid busy waiting areas.
NHS England have provided information regarding the learning disability register and the support it can provide. Please follow this link to find out more: Learning disabilities - NHS (www.nhs.uk)
ADHD
North Liverpool PCN LEAP ADHD Service
The LEAP ADHD Service receives referrals directly from Cheshire and Wirral Partnership (CWP) NHS Foundation Trust, providing a patient-centred approach to the care of adults with ADHD.
Our service offers comprehensive assessment, diagnosis, treatment initiation, and ongoing monitoring to support individuals in managing their condition effectively.
The multidisciplinary team is made up of Doctors, an Advanced Clinical Practitioner in Mental Health (ACP), and Neurodiversity Practitioners, all with specialist training and expertise in ADHD.
Please note: We do not accept direct referrals from any source other than CWP NHS Foundation Trust.
Enhanced Access
Local GP practices are working together to offer patients evening and weekend appointments, meaning you can see a GP, nurse or other health professional at a time which is most convenient for you.
We are here for you evenings and weekends. Please speak to your GP practice by phoning or speaking to the reception team for more information.
Weight Management Service
Please do not contact you practice regarding weight loss injections as surgeries are awaiting further local NHS guidance and places are limited due to funding.
Practices will contact eligible patients in due course.
Eligibility information can be found on the Cheshire & Merseyside ICB website.
We understand that some people may feel frustrated or disappointed if they are not eligible for medication-based treatments at this stage. Living with obesity can be emotionally and physically challenging, and it is completely normal to experience a range of feelings when seeking support for your health. If you are finding things difficult, NHS Talking Therapies offers free and confidential help for people who may be struggling with low mood, anxiety or other emotional pressures.
To find out more about obesity treatment and the support available on the NHS website.
If you are enrolled on the Weight Management Service, your participation is dependent on you attending a 13 session Behavioural Support Programme. This programme is essential in helping you manage your weight during and beyond the two-year medication course.
This programme will cover topics such as
· Nutrition
· Exercise
· Healthy Eating Habits
The sessions are available in person or online via Microsoft Teams and the programme’s app.
More information can be found
Mounjaro Technique, Tips and ADRs
Tirzepatide: What You Should Know
1. Hydration
Tirzepatide commonly reduces appetite, which can lead to people forgetting to drink enough.
· Aim for 1.5–2 litres of water per day unless advised otherwise.
· Staying hydrated helps reduce nausea, constipation, headaches, and dizziness.
· If vomiting or diarrhoea occur, sip oral rehydration solutions to replace electrolytes.
2. Micronutrient Deficiencies
Because people eat less on tirzepatide, their nutritional intake can drop.
· Patients should be aware of:
o Iron, B12, folate — risk increases with reduced red meat/greens intake or if they follow vegetarian/vegan diets.
o Vitamin D and calcium — especially important in darker months or if weight loss is rapid.
o Protein intake — aim for ~1.2–1.6 g/kg/day to minimise muscle loss.
· Tips:
o Consider a general multivitamin and vitamin D supplement.
o Include lean protein at each meal.
o Focus on high-nutrient foods: vegetables, fruit, whole grains, legumes, dairy/alternatives.
3. Common Side Effects
Most are mild and improve over time:
· Nausea, vomiting, acid reflux
· Constipation or diarrhoea
· Feeling full quickly
· Burping, sometimes with eggy/sulphur smell
· Mild injection-site reactions
· Hair loss
Lifestyle tips to reduce these:
· Eat smaller, slower meals.
· Avoid high-fat or heavy foods.
· Don’t lie down straight after eating.
· Keep well hydrated.
· Increase fibre gradually.
4. Red-Flag Side Effects (Seek Urgent Advice)
Patients should get medical help if they experience:
· Severe abdominal pain, especially radiating to the back
→ may indicate pancreatitis
· Signs of gallbladder problems: right-sided abdominal pain, fever, jaundice
· Persistent vomiting or inability to keep fluids down
· Signs of dehydration: dizziness, fainting, low urine output
· Severe allergic reaction: swelling, difficulty breathing, rash
5. General Lifestyle Tips
· Focus on nutrition quality, not just low calories.
· Aim for regular protein intake, ideally at each meal.
· Include high-fibre foods (fruit, vegetables, oats, pulses).
· Aim for regular movement: walking, strength training, stretching.
· Keep meals balanced and structured — skipping too many meals can worsen nausea.
· Limit alcohol: it can worsen GI symptoms and dehydration.
· Weigh yourself no more than once weekly to avoid discouragement during natural fluctuations.
· Prepare for dose escalation: symptoms often return briefly when increasing the dose.
6. Injection Technique
Please see the resources below for more information about injection technique and the medication in general.
· Troubleshooting Common Problems
· Eli Lilly Video on Injection Technique
Other Patient Resources
Newcastle North PCN Podcast Series
NHS Patient Webinars – Weight Management
NHS Digital Weight Management Programme